Vaccines. The Science. The Myths. The Legends.

Vaccine.
That word stirs up a lot of emotions, but even more so many questions that unless you go down the rabbit hole of understanding what a vaccine actually is and what it actually does, you’re left asking the same questions everyone else has:
“I got the flu vaccine, why did I still get the flu? “
To get to the bottom of this question, we need to first understand a few things.
- What is a vaccine?
- What is a virus?
- What are the different types of viruses?
- How many different types of vaccines are there and how do they work?
Once we have answers to these 4 questions, the information and misinformation light bulbs surrounding vaccines start to go off like furious lightning bolts.
Author’s Note:
“I sincerely enjoy writing these articles because it forces me to dive into deep research about topics I have a little previous knowledge about. After going through many article iterations, many times I find that my previous versions of data are faulty or need updating, or that I’ve been explaining things incorrectly. It’s a great way to keep myself up to date and on top of my own intellectual game. “
1. What is a Vaccine?
A vaccination is a treatment which makes the body stronger against an infection.
Let’s break that down for just a second.
A vaccination is a treatment, not always a cure. Those are two very different things. to take note of.
A vaccination makes the immune system stronger against an infection, but does not guarantee a life time immunity for every single person who gets it.
The body fights infections using the immune system, which is made up of millions upon millions of cells including T cells and B cells. An important part of the adaptive immune system is that it is much stronger when fighting a disease that it has already fought against before. Vaccination involves showing the immune system something which looks very similar to a particular virus or bacteria, which helps the immune system be stronger when it is fighting against the real infection.
I know there is some head scratching going on right now. I’m sure you’re asking the questions that popped into my head the first time I heard this statement.
“I got the polio vaccine, doesn’t that mean I’m totally immune to polio?
The short answer for this particular virus is, yes. You are totally immune to the 3 different strains of polio but for a reason you probably aren’t thinking of right now.
What what? 3 strains of polio?
That’s correct. But only 3. No more. Some viruses have many, many more, and some are constantly mutating.
When you get the polio vaccine, your body creates antibodies that are ready and prepared to fight the polio virus if it were to ever show it’s ugly head in your body.
The polio vaccine is a life long vaccine, and doesn’t need boosters to keep active in your body.
But the reason you are totally immune to polio isn’t because you got the vaccine. It’s because polio was eradicated through vaccines and herd immunity, so your body really never even has a chance to fight it again.
The vaccine caused that virus to all but disappear because less and less people were being infected due to having the vaccine, which means less and less chance for others to become infected.
Eventually, polio became a non-issue for most countries.
Note: There are still some cases of polio in the world today, albeit very few. In 2017 there were 22 reported cases world wide.
Polio Disease and Poliovirus
There are three wild types of poliovirus (WPV) – type 1, type 2, and type 3. People need to be protected against all three types of the virus in order to prevent polio disease and the polio vaccination is the best protection. There are two vaccines used to protect against polio disease, oral polio vaccine and inactivated poliovirus vaccine.
To protect yourself against the polio disease you need to get 3 different vaccinations to ensure you are protected against all strains.
This brings us to our next point – Understanding what a virus is.
2. What is a Virus?
Viruses are microscopic parasites, generally much smaller than bacteria. They lack the capacity to thrive and reproduce outside of a host body.
Viruses cannot reproduce on their own, they require a host cell to attach to and they then inject their RNA into the host cell which programs the cell to start creating replicas of the virus, instead of making copies of of itself.
You see, all things have a need to reproduce, even things not considered alive, like a virus. Viruses cannot reproduce asexually, on their own, or without a host cell.
The primary role of the virus or virion is to “deliver its DNA or RNA genome into the host cell so that the genome can be expressed.
First, viruses need to access the inside of a host’s body. Respiratory passages and open wounds can act as gateways for viruses. Sometimes insects provide the mode of entry.
Certain viruses will hitch a ride in an insect’s saliva and enter the host’s body after the insect bites. Examples include the viruses that cause yellow fever, malaria, and dengue fever.
Viruses will then attach themselves to host cell surfaces. They do so by recognizing and binding to cell surface receptors, like two interlocking puzzle pieces. Many different viruses can bind to the same receptor and a single virus can bind to different cell surface receptors. While viruses use them to their advantage, cell surface receptors are actually designed to serve the cell.
After a virus binds to the surface of the host cell, it can start to move across the outer covering or membrane of the host cell. There are many different modes of entry.
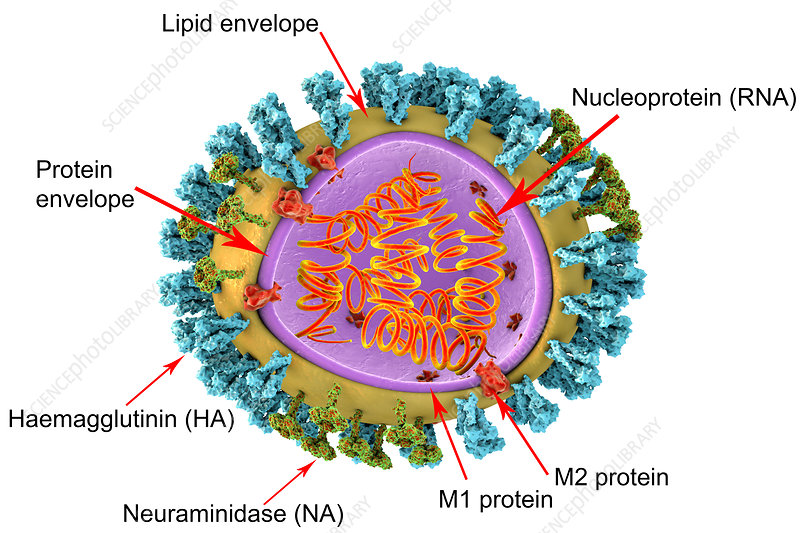
HIV, a virus with an envelope, fuses with the membrane and is pushed through. Another enveloped virus, the influenza virus, is engulfed by the cell. Some non-enveloped viruses, such as the polio virus, create a porous channel of entry and burrow through the membrane.
This is what makes coming up with a vaccine so difficult. There are different kinds of viruses, that enter the body in different ways, attach to different types of cells, in different kinds of ways.
Later, we’ll talk about the different types of vaccines for the different types of viruses.
Vaccine. Starting to see why it’s not a one-size-fits-all kind of word anymore, right?
Once inside, viruses release their genomes and also disrupt or hijack various parts of the cellular machinery. Viral genomes direct host cells to ultimately produce viral proteins (many a time halting the synthesis of any RNA and proteins that the host cell can use).
3. What are the different kinds of viruses?
Here’s where things start to get tricky. In an attempt to not bore you with paragraphs upon paragraphs of scientific jargon and crazy explanations for each one, I’ve consolidated the different types in easy to read nomenclature below.
First let’s define a few words:
——————————————————-
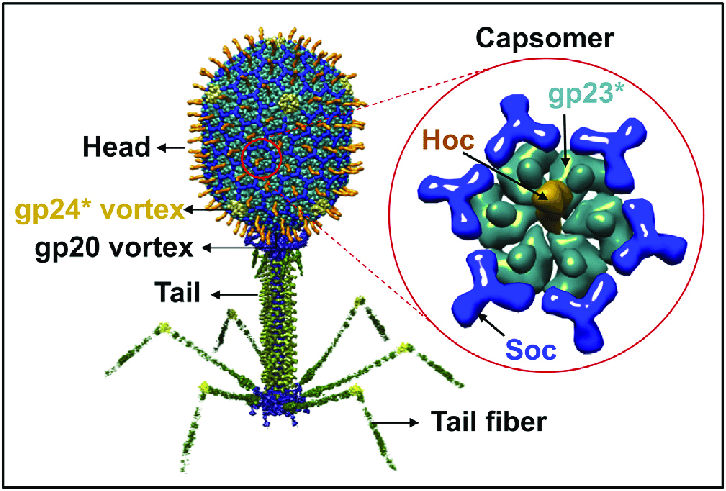
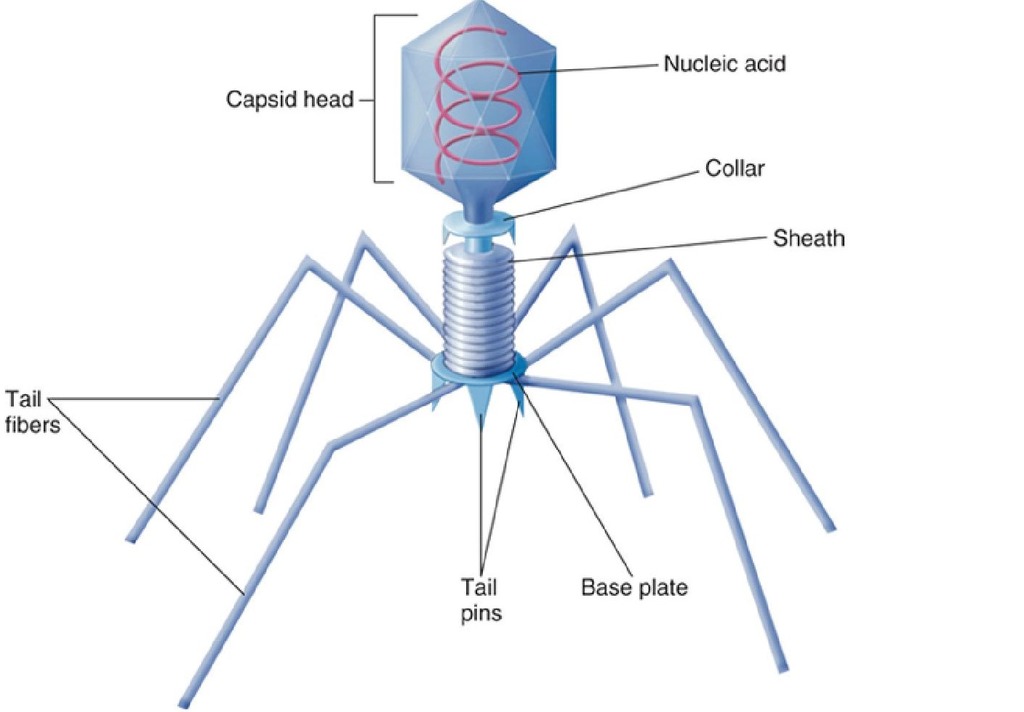
Capsomer:
The capsomer is the out protein covering of a virus. All viruses have them, they have different properties, some have many different types surrounding them, but, thankfully, because they are protein based they are susceptible to heat and you may have guessed it – Soap.
Info: The nano-abrasive particles in soap that form the soap bubbles along with heated water basically melt away that outer covering. Melt away a virus’s “skin” and all the insides come pouring out.
Next time you wash your hands you can think of all the nasty viruses you are essentially disemboweling. Neat huh?
Virion:
Virion is a fully formed virus that is able to infect.
——————————————————-
Different Types of Viruses
Helical
These viruses are composed of a single type of capsomere stacked around a central axis to form a helical structure, which may have a central cavity, or tube. The well-studied tobacco mosaic virus is an example of a helical virus.
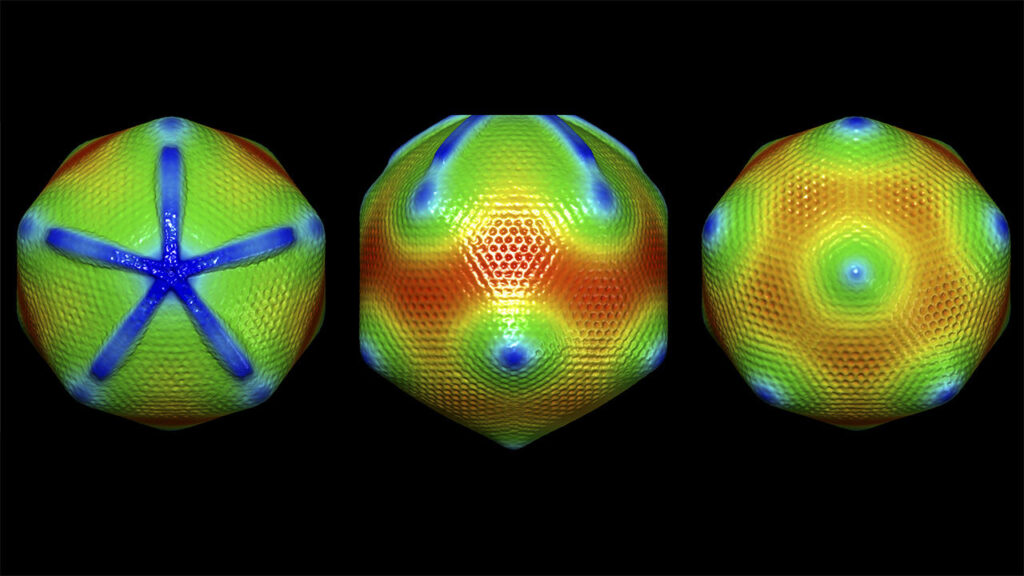
Icosahedral
ost animal viruses are icosahedral or near-spherical with chiral icosahedral symmetry. Many viruses, such as rotavirus, have more than 60 capsomers and appear spherical but they retain this symmetry.

Envelope
Some species of virus envelop themselves in a modified form of one of the cell membranes, either the outer membrane surrounding an infected host cell or internal membranes such as nuclear membrane or endoplasmic reticulum, thus gaining an outer lipid bilayer known as a viral envelope. This membrane is studded with proteins coded for by the viral genome and host genome; the lipid membrane itself and any carbohydrates present originate entirely from the host.
The influenza virus and HIV use this strategy. Most enveloped viruses are dependent on the envelope for their infectivity.
Complex
The poxviruses are large, complex viruses that have an unusual morphology. The viral genome is associated with proteins within a central disc structure known as a nucleoid.
Giant viruses
Mimivirus is one of the largest characterised viruses, with a capsid diameter of 400 nm.
Some viruses that infect Archaea, or single celled organisms, have complex structures unrelated to any other form of virus, with a wide variety of unusual shapes, ranging from spindle-shaped structures to viruses that resemble hooked rods, teardrops or even bottles.
Whew, ok, so now we know there are loads of different styles of virus now lets look at the different ways they can replicate:
Genome replication
The genetic material within virus particles, and the method by which the material is replicated, varies considerably between different types of viruses.
DNA viruses
The genome replication of most DNA viruses takes place in the cell’s nucleus.
RNA viruses
RNA replication usually takes place in the cytoplasm.
All RNA viruses use their own RNA replicase enzymes to create copies of their genomes.
Reverse transcribing viruses
Reverse transcribing viruses have ssRNA (Retroviridae, Metaviridae, Pseudoviridae) or dsDNA (Caulimoviridae, and Hepadnaviridae) in their particles. Reverse transcribing viruses with RNA genomes (retroviruses) use a DNA intermediate to replicate, whereas those with DNA genomes (pararetroviruses) use an RNA intermediate during genome replication.
You are starting to see, coming up with a vaccine might not be so simple. Below, I’ve copied a chart from wikipedia to show the different genomes and viral types of many known viruses you may have heard of. Each of these different things combine to make it exceedingly hard to come up with a vaccine for any one type of virus, and we haven’t even brushed the surface of viral strains and mutations.
Check out the info areas below with dramatic effect!
DNA viruses
Further information: DNA virus
- Group I: viruses possess double-stranded DNA. Viruses that cause chickenpox and herpes are found here.
- Group II: viruses possess single-stranded DNA.
| Virus family | Examples (common names) | Virion naked/enveloped | Capsid symmetry | Nucleic acid type | Group |
|---|---|---|---|---|---|
| 1. Adenoviridae | canine hepatitis virus | Naked | Icosahedral | ds | I |
| 2. Papovaviridae | Papillomavirus, polyomaviridae, simian vacuolating virus | Naked | Icosahedral | ds circular | I |
| 3. Parvoviridae | Parvovirus B19, canine parvovirus | Naked | Icosahedral | ss | II |
| 4. Herpesviridae | Herpes simplex virus, varicella-zoster virus, cytomegalovirus, Epstein–Barr virus | Enveloped | Icosahedral | ds | I |
| 5. Poxviridae | Smallpox virus, cow pox virus, sheep pox virus, orf virus, monkey pox virus, vaccinia virus | Complex coats | Complex | ds | I |
| 6. Anelloviridae | Torque teno virus | Naked | Icosahedral | ss circular | II |
| 7. Pleolipoviridae | HHPV1, HRPV1, HGPV1, His2V | Enveloped | ss/ds linear/circular | I/II |
RNA viruses
Further information: RNA virus
- Group III: viruses possess double-stranded RNA genomes, e.g. rotavirus.
- Group IV: viruses possess positive-sense single-stranded RNA genomes. Many well known viruses are found in this group, including the picornaviruses (which is a family of viruses that includes well-known viruses like Hepatitis A virus, enteroviruses, rhinoviruses, poliovirus, and foot-and-mouth virus), SARS virus, hepatitis C virus, yellow fever virus, and rubella virus.
- Group V: viruses possess negative-sense single-stranded RNA genomes. Ebola and Marburg viruses are well known members of this group, along with influenza virus, measles, mumps and rabies.
Reverse transcribing viruses
- Group VI: viruses possess single-stranded RNA viruses that replicate through a DNA intermediate. The retroviruses are included in this group, of which HIV is a member.
- Group VII: viruses possess double-stranded DNA genomes and replicate using reverse transcriptase. The hepatitis B virus can be found in this group.
| Virus Family | Examples (common names) | Capsid naked/enveloped | Capsid Symmetry | Nucleic acid type | Group |
|---|---|---|---|---|---|
| 1. Retroviridae | HIV | Enveloped | dimer RNA | VI | |
| 2. Caulimoviridae | Caulimovirus, Cacao swollen-shoot virus (CSSV) | Naked | VII | ||
| 3. Hepadnaviridae | Hepatitis B virus | Enveloped | Icosahedral | circular, partially ds | VII |
As you may have guessed, each one of these types of viruses requires a different kind of tool set to create a vaccine.
Now that you’re overly informed on the different types of viruses, and are getting some semblance on how difficult it might be to create a vaccine for each one, not to mention the possibility of different strains of each one, let’s discuss the different types of vaccines, and how each one is effective or less effective in their own ways.
4. How many different types of vaccines are there?
There are several different types of vaccines. Each type is designed to teach your immune system how to fight off certain kinds of viruses— and the serious diseases they can cause.
Some viruses respond better to certain types of vaccines, while some of the more effective vaccines take longer to create and test.
When scientists create vaccines, they consider:
- How your immune system responds to the virus
- Who needs to be vaccinated against the virus
- The best technology or approach to create the vaccine
- What type of virus they are dealing with
Based on a number of these factors, scientists decide which type of vaccine they will make. There are 4 main types of vaccines:
- Live-attenuated vaccines
- Inactivated vaccines
- Subunit, recombinant, polysaccharide, and conjugate vaccines
- Toxoid vaccines
Live-attenuated vaccines
Live vaccines use a weakened (or attenuated) form of the germ that causes a disease.
Because these vaccines are so similar to the natural infection that they help prevent, they create a strong and long-lasting immune response. Just 1 or 2 doses of most live vaccines can give you a lifetime of protection against a germ and the disease it causes.
But live vaccines also have some limitations. For example:
- Because they contain a small amount of the weakened live virus, some people should talk to their health care provider before receiving them, such as people with weakened immune systems, long-term health problems, or people who’ve had an organ transplant.
- They need to be kept cool, so they don’t travel well. That means they can’t be used in countries with limited access to refrigerators.
- They can have adverse effects in certain people which causes hyper immune response or the possibility of an allergic reaction.
Live vaccines are used to protect against:
- Measles, mumps, rubella (MMR combined vaccine)
- Rotavirus
- Smallpox
- Chickenpox
- Yellow fever
Inactivated vaccines
Inactivated vaccines use the killed version of the germ that causes a disease.
Inactivated vaccines usually don’t provide immunity (protection) that’s as strong as live vaccines. So you may need several doses over time (booster shots) in order to get ongoing immunity against diseases.
Inactivated vaccines are used to protect against:
- Hepatitis A
- Flu (shot only)
- Polio (shot only)
- Rabies
Subunit, recombinant, polysaccharide, and conjugate vaccines
Subunit, recombinant, polysaccharide, and conjugate vaccines use specific pieces of the germ — like its protein, sugar, or capsid (a casing around the germ).
Basically, these vaccines are created using the outer protective coating (capsomer) as a map, with nothing on the inside.
A protein walnut shell with no nut if you will.
Because these vaccines use only specific pieces of the virus, they give a very strong immune response that’s targeted to key parts of the virus. They can also be used on almost everyone who needs them, including people with weakened immune systems and long-term health problems.
One limitation of these vaccines is that you may need booster shots to get ongoing protection against diseases.
These vaccines are used to protect against:
- Hib (Haemophilus influenzae type b) disease
- Hepatitis B
- HPV (Human papillomavirus)
- Whooping cough (part of the DTaP combined vaccine)
- Pneumococcal disease
- Meningococcal disease
- Shingles
Toxoid vaccines
Toxoid vaccines use a toxin (harmful product) made by the virus that causes a disease. They create immunity to the parts of the virus that cause a disease instead of the virus itself. That means the immune response is targeted to the toxin instead of the whole virus.
Like some other types of vaccines, you may need booster shots to get ongoing protection against diseases.
Toxoid vaccines are used to protect against:
HOLY CRAP. TOO MUCH INFO.
Yup. There’s a lot. And here’s another monkey wrench to throw into the scenario.
Strains.
Different viruses can have different strains associated with them. As mentioned above, the Polio virus, for example, has 3 different types of strains. This means you need to come up with a vaccine for each strain. And each strain might not react the same to each type of vaccine created.
The good news is, not all viruses constantly mutate. So if you can isolate the strains initially, and create a vaccine, then essentially, you will eventually cure the world of that virus, or the disease that is causes.
Now let’s get to the virus that everyone knows and loves – Influenza.
1.) “Why do I get the flu when I get the flu vaccine?”
2.) “I’ve never had the flu vaccine, and have never had the flu. So why do I need it?”
So the flu is is a pesky virus for the simple fact that not only are there many strains of the virus, but there are multiple sub-types that are also always at work changing, mutating, and becoming non-receptive to different vaccines that scientists come up with.
There are 18 different HA subtypes and 11 different NA subtypes. Subtypes are named by combining the H and N numbers – e.g., A(H1N1), A(H3N2).
There are four types of influenza viruses: A, B, C and D
A and B type are generally what make us sick, although, C and D can also cause some reaction in certain individuals.
So you can take 18 different HA types, and combine them with 11 different NA types, along with a slew of other variables that come along with viral lineage, and all the sudden you have literally thousands of different possibilities that this virus could take form in throughout the flu season.
Generally, scientist pick 4 of these that they think will be prominent during that particular season for a number of reasons, and this will b e the “flu shot” you get during flu season.
See the problem here?
Now the mind is working.
“So you’re saying there could be over a 1000 different variations of the flu, and we pick a select few and hope for the best?”
Yup. And they do a darn good job of it for the most part as well.
Sometimes though, they get it wrong.
The overall burden of influenza for the 2017-2018 season was an estimated 45 million influenza illnesses, 21 million influenza-associated medical visits, 810,000 influenza-related hospitalizations, and 61,000 influenza-associated deaths
Compared to the 2018-2019 season which killed around 35,000 people in the United States, and you can see how picking the wrong chain of vaccines for the year can have an effect on the outcome that season.
So let’s address those questions again:
1.) “Why do I get the flu when I get the flu vaccine?”
Any time you get a vaccine, you will have a reaction. Your body is basically declaring a fake war inside of you when the vaccine enters your body. Some people will react mildly, and others will react in a more aggressive fashion.
Basically, you may not have gotten the flu, you might have just had a bad reaction to that vaccine.
Or, you got a strain of the flu that wasn’t in the vaccine. Knowing how many there are, and knowing that scientists sometimes get it wrong, it’s very common for people in certain areas to have different strains of the flu than other parts of the country.
2.) “I’ve never had the flu vaccine, and have never had the flu. So why do I need it?”
I tend to be skeptical of this questions because frankly, how would one know if they’ve ever had the flu? Unless you’re tested for it at the Doctor for the antigen, how would you know if you’ve had it or not?
Have you ever been sick? Could have been the flu.
Some people have mild cases of the flu, which have more cold like symptoms.
Maybe you have an outstanding immune system and when your body gets infected, it immediately takes action and you don’t have harsh symptoms like other people.
Maybe you’re just really, really lucky.
Let’s address a follow up question before ending the article.
Why should I get the flu shot if I’ve never been sick with the flu and don’t think I need it?
Remember before how we discussed how certain types of vaccines provide different types of immunity and different lengths of immunity?
The flu vaccines are the same thing.
Perhaps one year you get the flu shot, and you get sick with a strain that wasn’t in the vaccine that season.
But the following season, a new vaccine comes out with different strains, but the strains that were included in the last season’s vaccine are prominent.
Guess what? You’re immune to that strain.
You read correctly. You can stack vaccines so that eventually, you’re almost nearly covered for any strain that might come your way! Cool, right?
This immunity doesn’t usually last forever, the main consensus is about 5 years, but it can vary from person to person.
So if every person in the United States were to get the flu shot every single year, within less than a decade, you’d be seeing much less flu cases, more herd immunity to the flu, and less strains popping up due to the inability for them to infect people and mutate.
The flu vaccine is a personal choice. But some Vaccines when not taken can bring back extremely deadly diseases that were once thought eradicated.
In my next article, I’ll be going over my opinions on vaccines, how they are administered and how that process can be improved, and I’ll address vaccine side effects, the autism question, and how we can better serve humanity with better versions of vaccines.
I’ll also be addressing a very sensitive topic.
Vaxxers vs Anti-Vaxxers. Who’s really right?
Insider hint: I have cases for both sides. You be the judge.
When we think in absolutes our minds become dull.
Vaccines are a wonderful medical tool but there are obvious risks for a small percentage of the population that need to be addressed before we can expect everyone to embrace vaccines without question.
Understanding vaccine science while at the same time understanding this this fact will help eradicate misinformation and help us get back on track to conquering viruses and diseases for all mankind.
Recent Comments